Gestational Trophoblastic Disease
Understanding Gestational Trophoblastic Disease (GTD): What You Need to Know
A group of unusual illnesses linked to pregnancy, known as Gestational Trophoblastic Disease (GTD), are quite rare. These stem from those cells that make the early placenta, also known as trophoblastic cells. When these cells grow oddly, it causes these diseases - they can be harmless to harmful. The harmful ones are also known as Gestational Trophoblastic Neoplasia (GTN). We dive deep into these rare disorders in this blog. Here, we'll discuss what might cause them, their variety, signs to look out for, how they're diagnosed and treated, and what to expect moving forward with this condition.
Book an Appointment
What is Gestational Trophoblastic Disease?
There's a set of conditions called Gestational Trophoblastic Disease, or GTD. This disorder affects how the trophoblastic tissue grows. This tissue is vital for embryo development. Some examples of GTD and GTN are molar pregnancy, a benign condition, and choriocarcinoma, a serious form of cancer respectively. Fortunately, most GTD cases can be cured. If ignored, though, some can harm our health badly by developing into GTN. Catching GTD early and taking action stops problems and makes therapy work well.
Types of Gestational Trophoblastic Disease
GTD can be broadly categorized into benign and malignant types. The malignant types are also referred to as GTN.
1. Benign Conditions
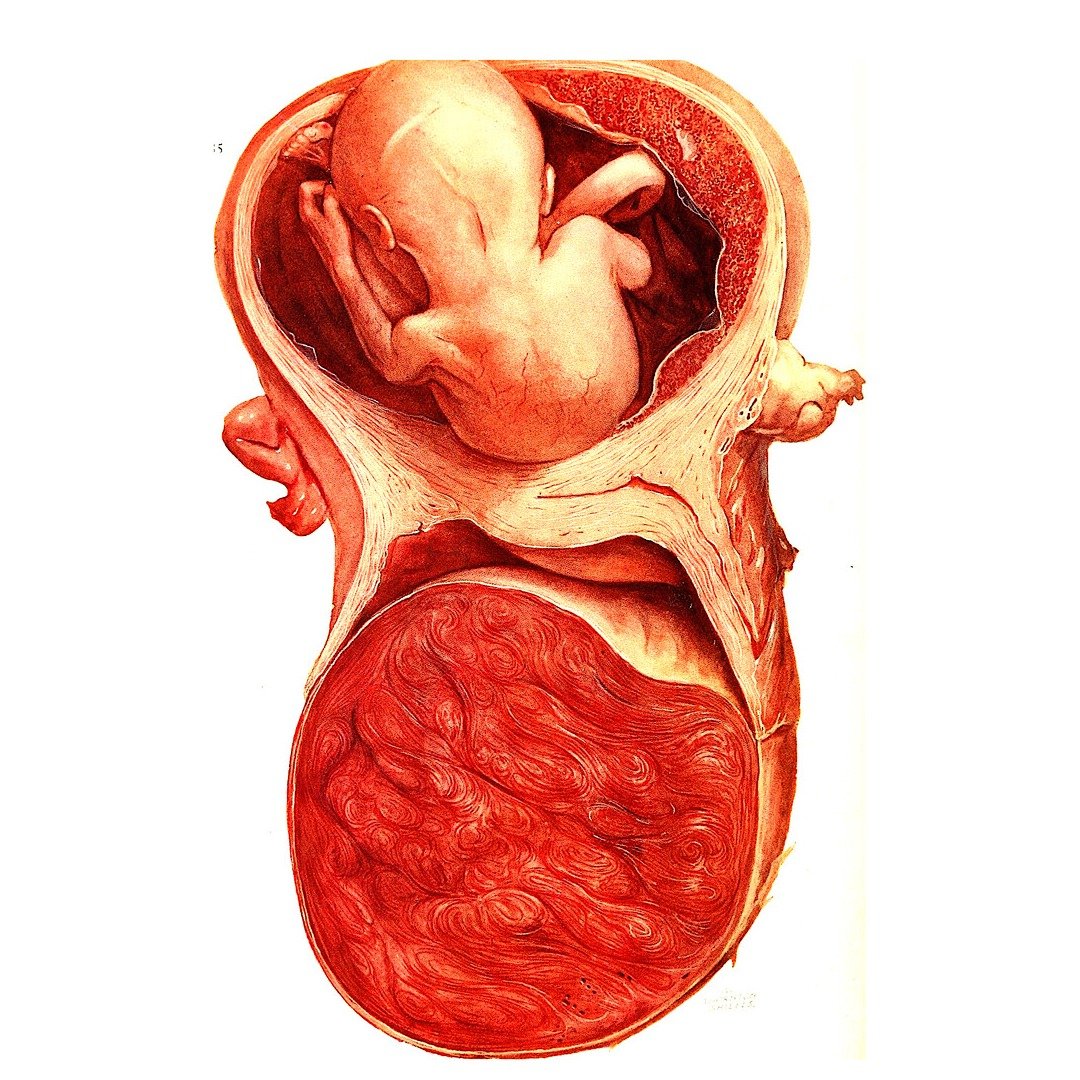
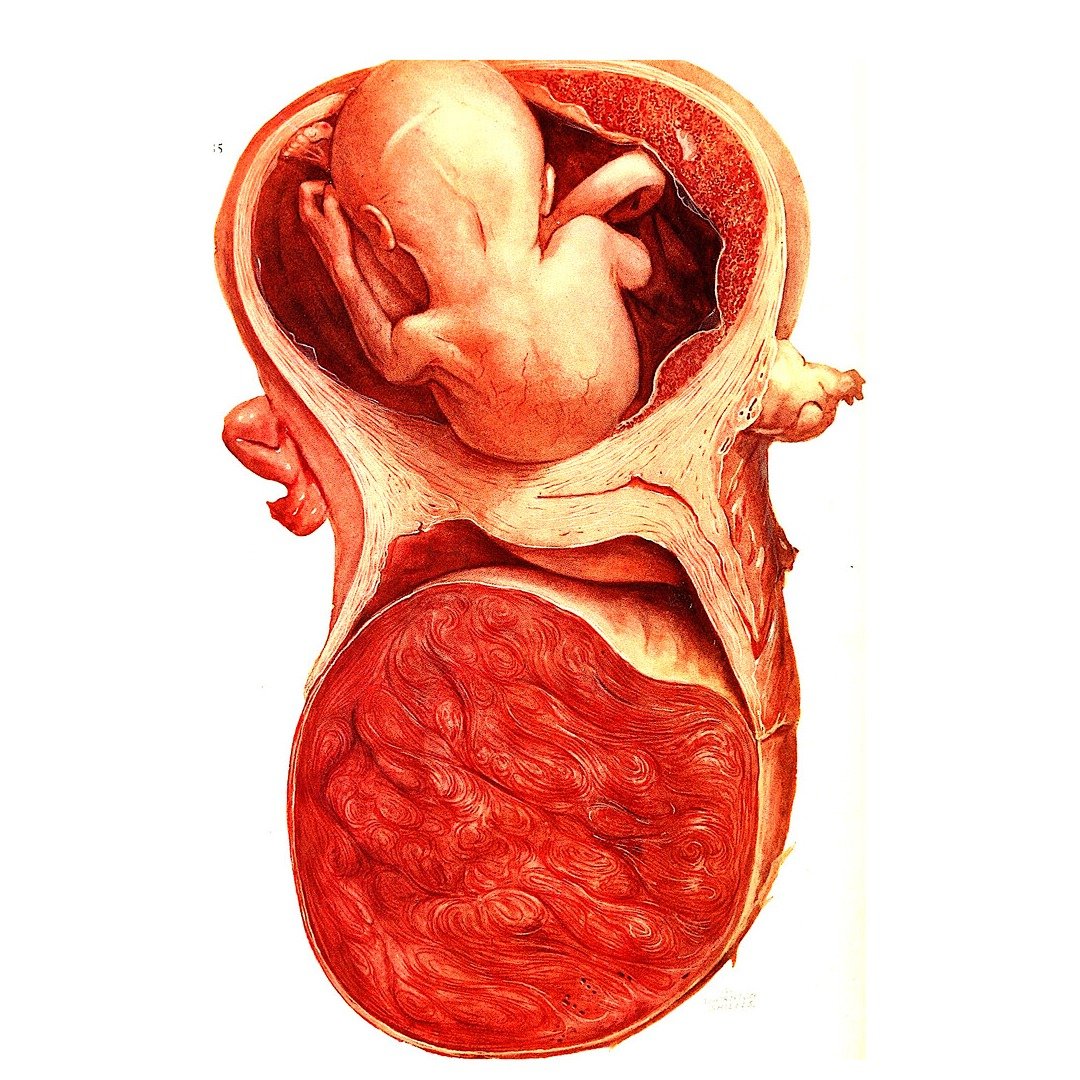
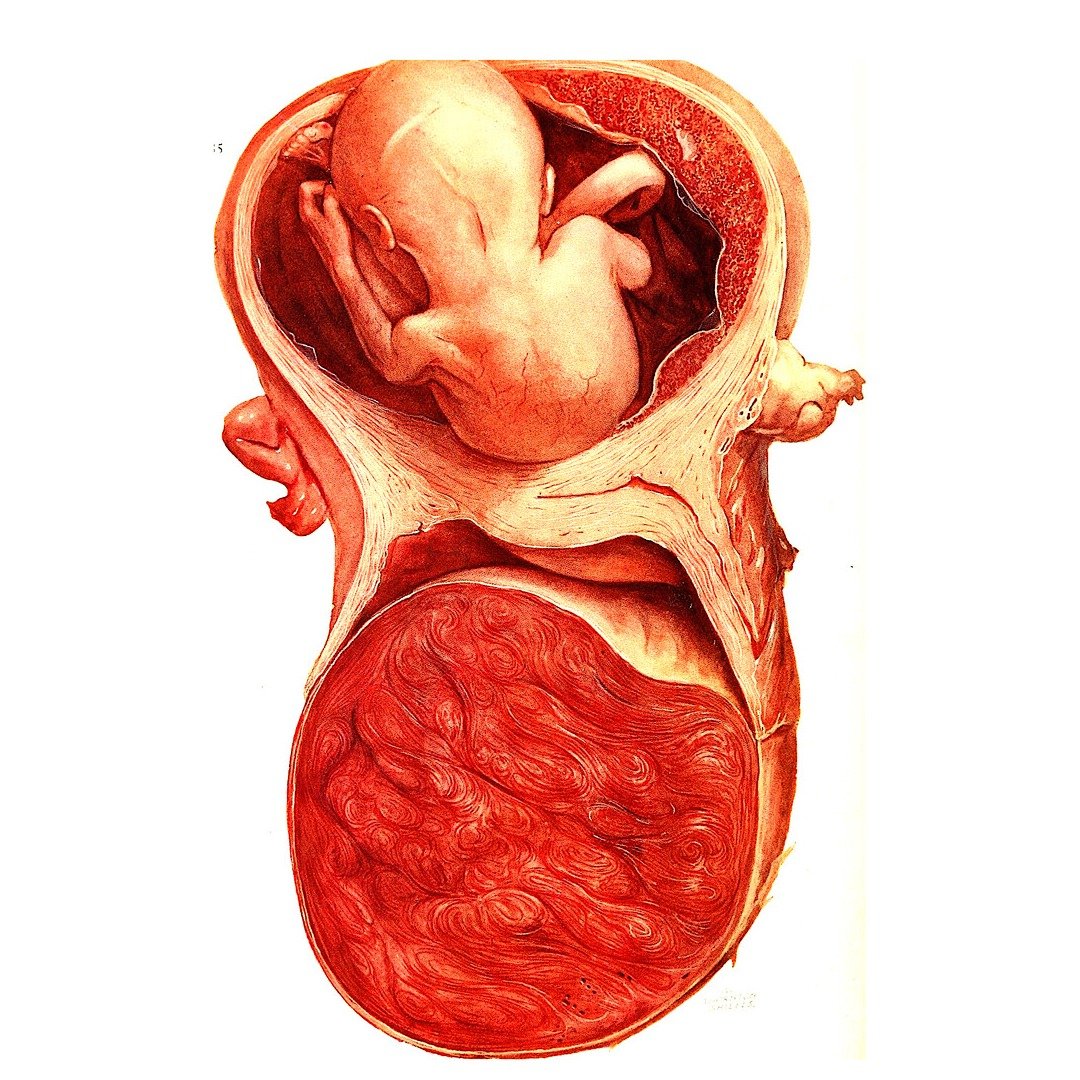
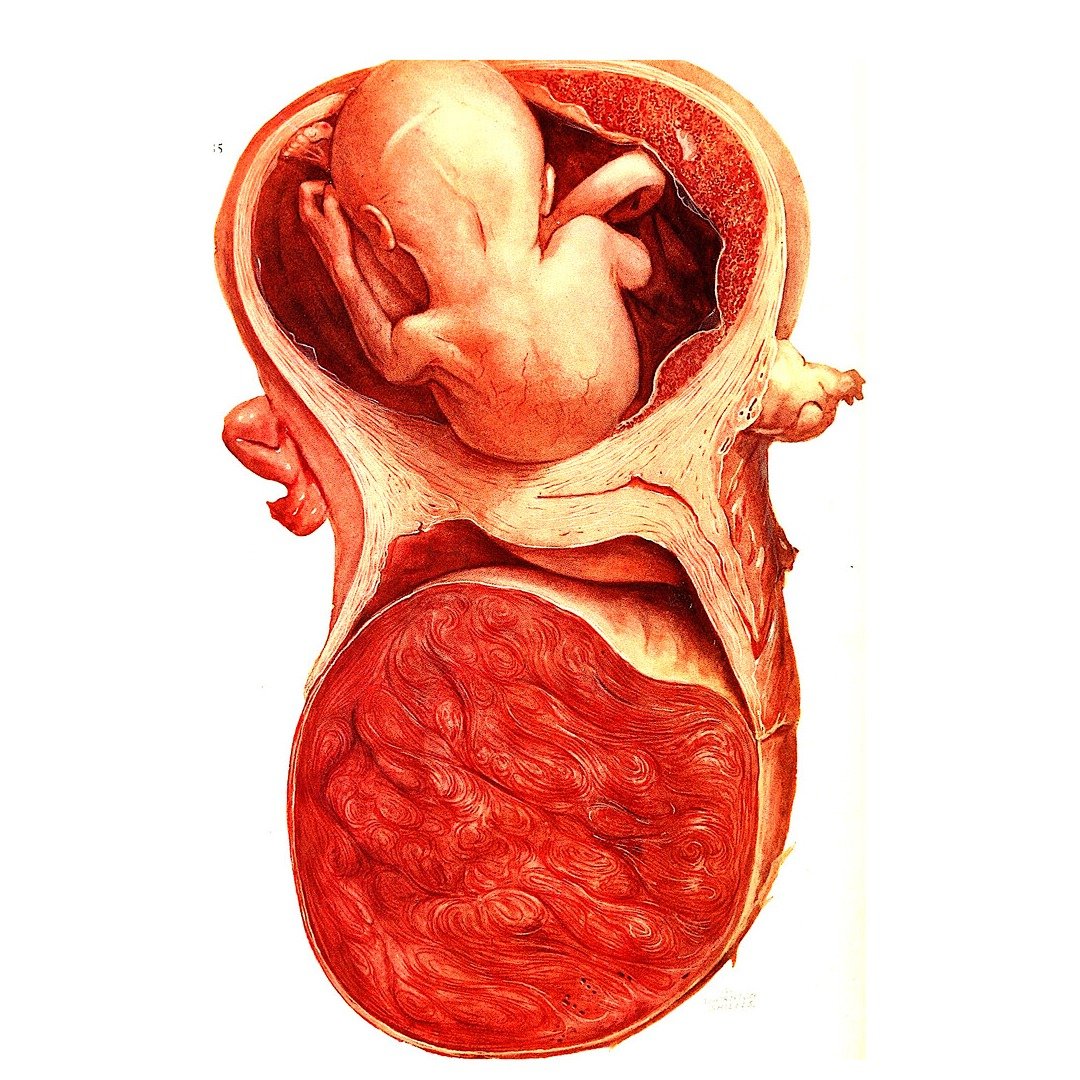
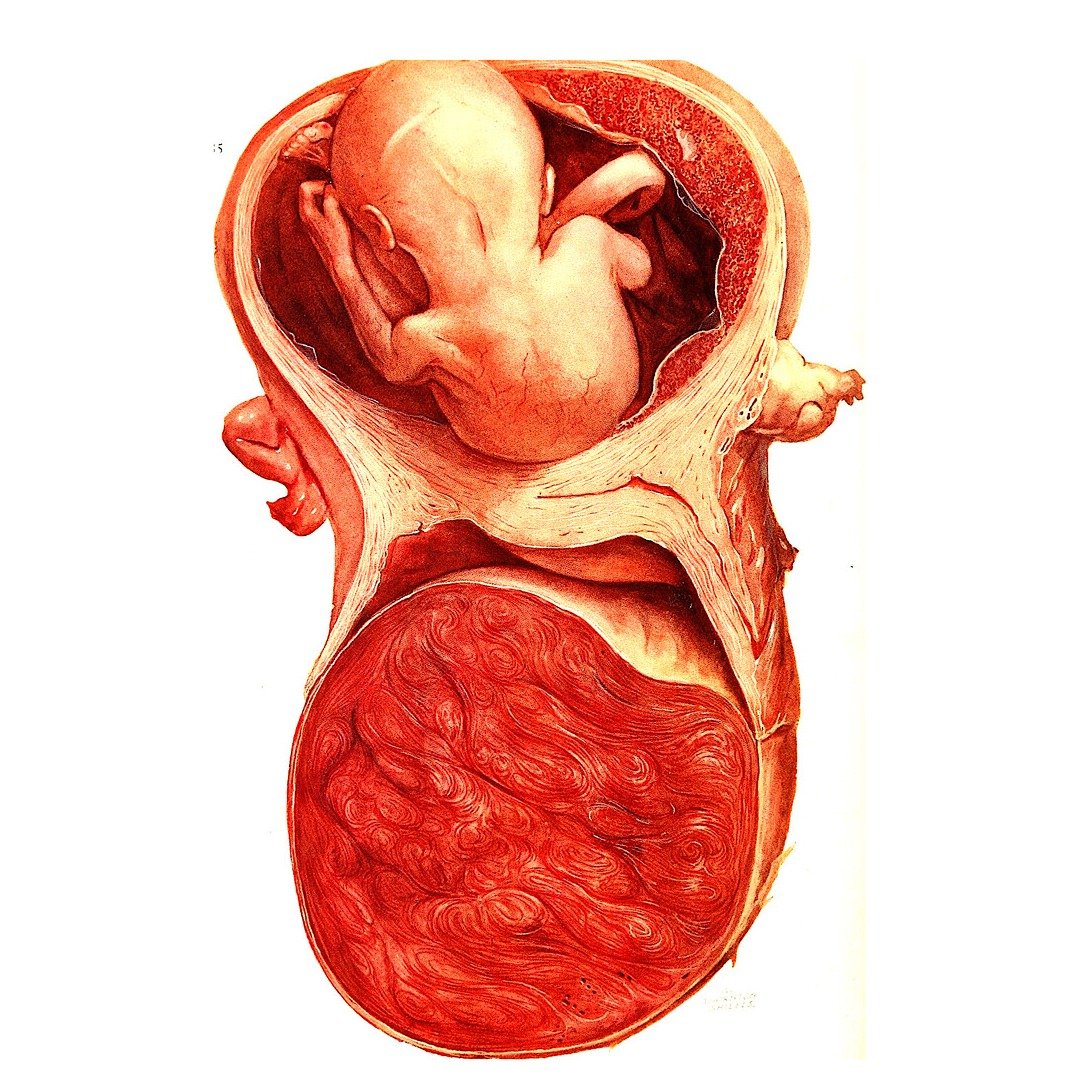
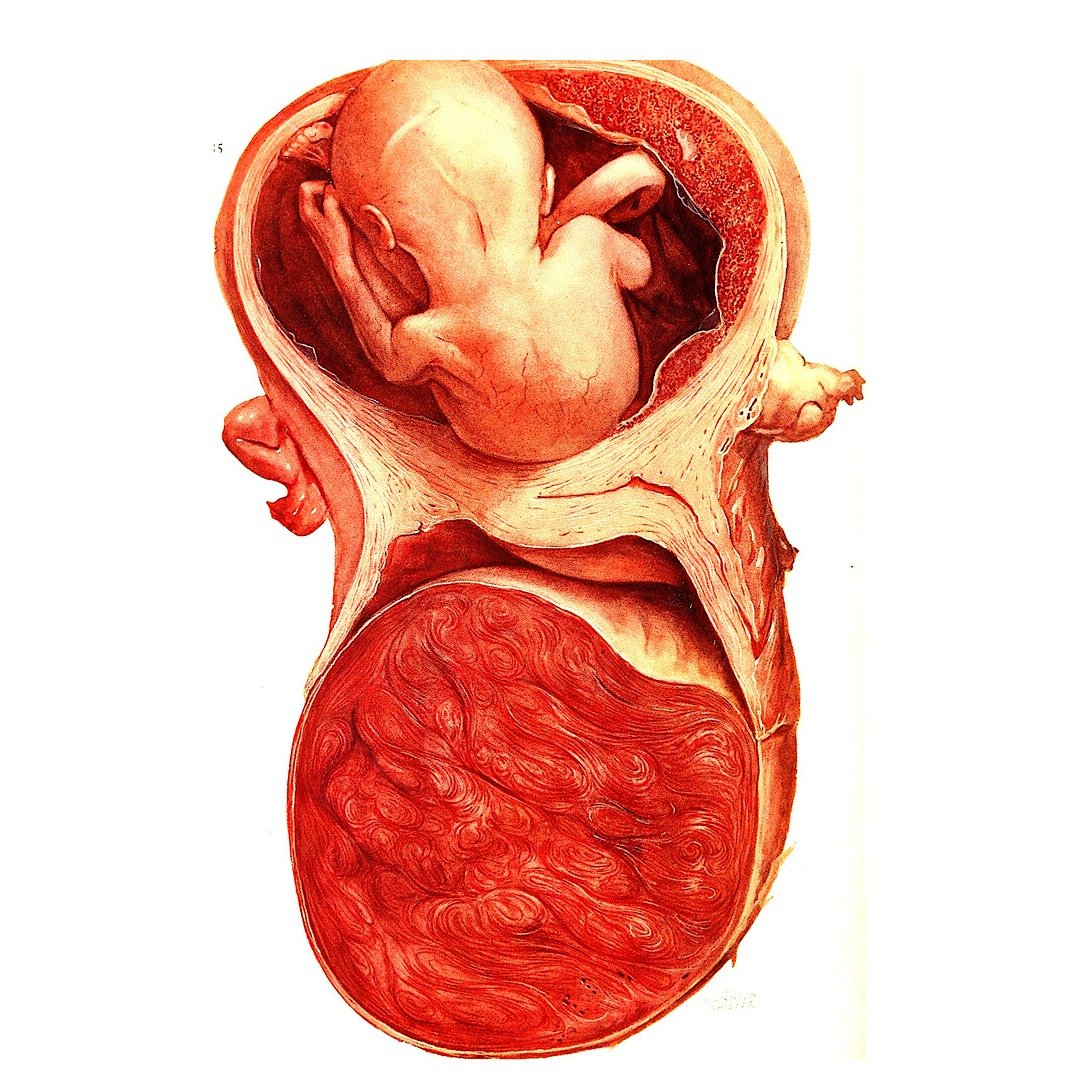
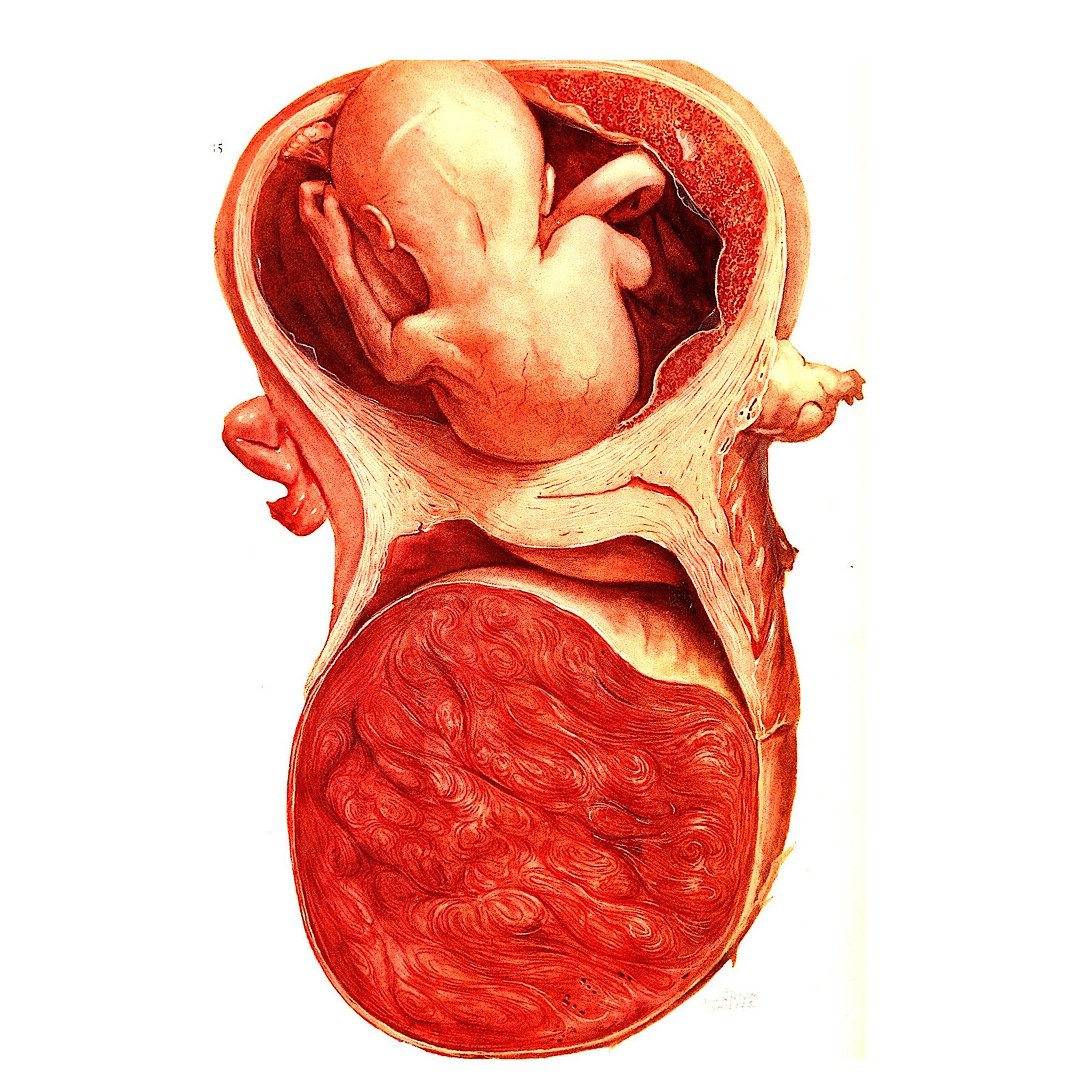
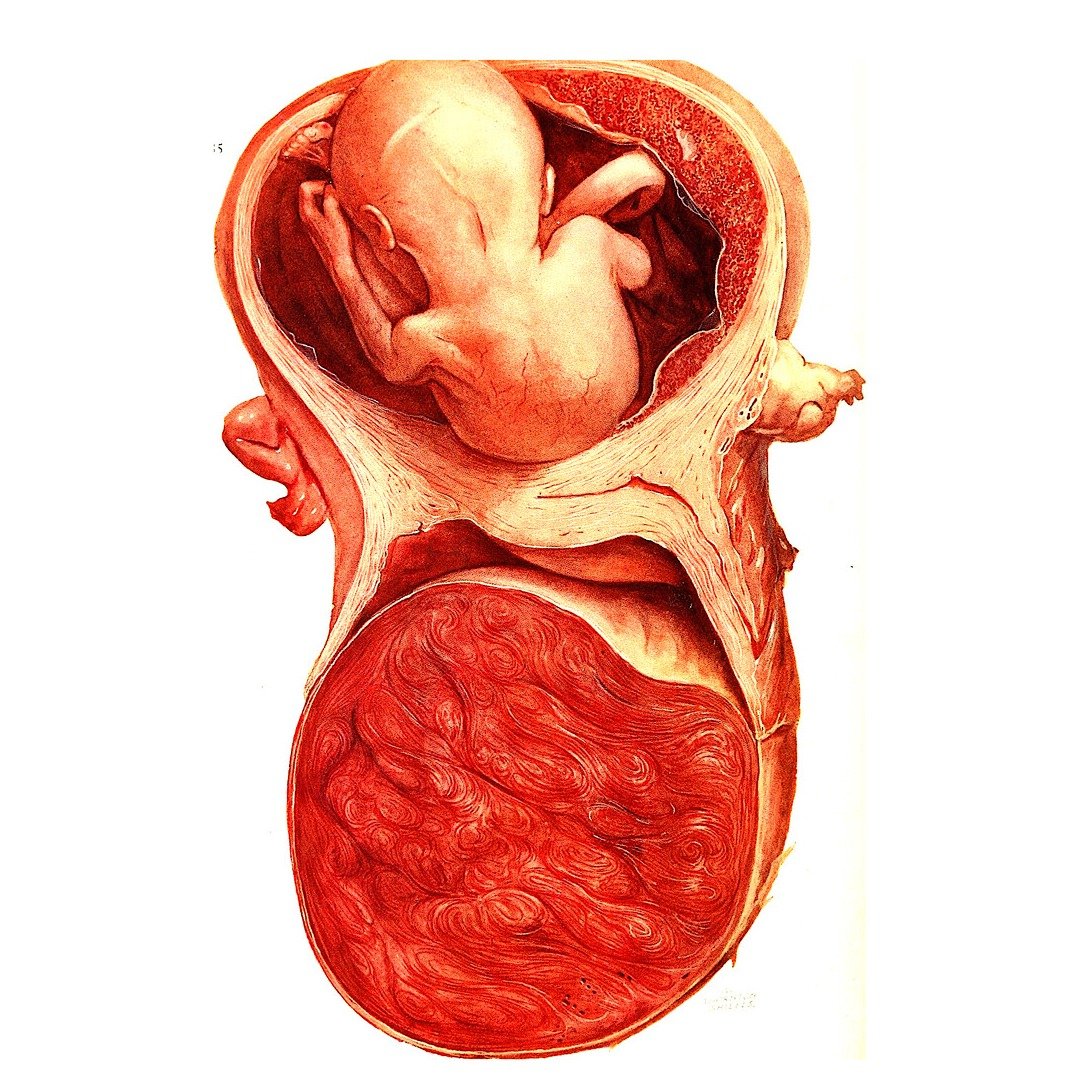
Complete Hydatidiform Mole (CHM): It happens when a sperm fertilizes an egg that lacks mother's DNA. This leads to a peculiar placenta, brimming with cysts that look like a grape bunch. No healthful baby can grow from a complete mole, as there's no viable fetus.
A Partial Hydatidiform Mole, or PHM, happens when an egg gets fertilized by either two sperm or just one duplicating its chromosomes. Even though some tiny bits of fetal tissue might be there, they usually can't survive. So, a healthy pregnancy won't happen.
2. Malignant Conditions or GTN
Invasive Mole: An invasive mole is when a type of growth called a hydatidiform mole burrows into the wall of the womb. This can cause issues like a tearing womb and may demand stronger treatment.
Choriocarcinoma: Choriocarcinoma is a very uncommon, fierce cancer that begins from trophoblastic tissue. It can move swiftly to other areas like the lungs, liver, or brain.
Placental-Site Trophoblastic Tumor (PSTT): A Placental-Site Trophoblastic Tumor, or PSTT, is an extremely rare type that starts where the placenta implants itself. Although it grows at a slow pace, it can still reach other organs.
Epithelioid Trophoblastic Tumor (ETT): ETT is a less frequent but more aggressive variant. Its hallmark is aggressive behavior and the potential to spread, much like a PSTT
Causes and Risk Factors of Gestational Trophoblastic Disease
Gestational Trophoblastic Disease: What Causes It and Who's at Risk? GTD has causes that remain unknown. But, some risk factors increase your chances of facing this issue:
Age: If you are under 20 or over 35 years, GTD could be a concern. The likelihood is higher for complete hydatidiform moles.
Previous Molar Pregnancy: Had a molar pregnancy before? The chance of another molar pregnancy and GTD goes up.
Ethnicity: GTD appears more in certain ethnic groups, particularly Asian women, pointing to possible genetic and environmental influences.
Nutritional Deficiencies: Women with lower carotene and vitamin A levels might be more at risk. Why? These nutritional factors can affect how cells grow, especially trophoblastic tissue
Book an Appointment
Gestational Trophoblastic Disease Symptoms
Gestational Trophoblastic Disease showcases peculiar signs. These can shift according to the disease type and stage, like:
Vaginal Bleeding: Continual, unusual heavy bleeding during or after pregnancy.
Excessive Nausea and Vomiting: Feeling sick too often or throwing up a lot, a condition called hyperemesis gravidarum, because of high hCG (pregnancy hormone) levels.
Pelvic Pain or Pressure: Pain or pressure in the lower belly or pelvis, mostly due to changes in the size of the uterus.
Rapid Uterine Enlargement: The uterus growing too fast for the present time and age of pregnancy.
Passage of Grape-like Tissue: Sometimes, patients might discharge tissue from their private parts that appears like a bunch of grapes
How is Gestational Trophoblastic Disease Diagnosed
Identifying Gestational Trophoblastic Disease (GTD) needs a careful process. This combines checking out a patient, doing lab tests, and using special picture-taking methods. The aim? To confirm if GTD is present and to know its kind and size.
Medical History and Physical Examination:
First, doctors take a careful look at symptoms like irregular bleeding. They also do a check of the pelvis to spot unusual uterine changes like irregular or enlarged size.
hCG Blood Test:
A hormone called human chorionic gonadotropin (hCG), usually linked with pregnancy, shows up at very high levels. This is an important sign to diagnose the condition. If these hCG levels stay high, it often points to GTD.
Ultrasound Imaging:
In figuring out molar pregnancies, performing an ultrasound is key. This test can show unusual patterns like a "snowstorm" or "grape-like bunch" linked with hydatidiform moles.
Histopathological Examination:
Tissue samples obtained through uterine evacuation are analyzed under a microscope. This step is critical for distinguishing between benign and malignant GTD forms.
Additional Imaging:
In cases where malignant GTD is believed, high-tech scanning such as CTs, MRIs or chest X-rays are done to spot spread and organize care.
Gestational Trophoblastic Disease Treatment
The GTD type, disease severity, and future family plans guide treatment choices. Spotting early and proper treatment greatly helps.
1. Treatment for Benign GTD (Hydatidiform Mole)
Uterine Evacuation:
Your go-to solution is Suction Evacuation of uterine contents. It's a process that gets rid of the molar tissue in the uterus. We mostly do it under general anesthesia. Why? To make sure we remove all the odd tissue. And to cut down on problems like puncturing the uterus.
hCG Monitoring:
After uterine evacuation, we keep an eye on human chorionic gonadotropin (hCG) levels. If these numbers stay high after treatment, it could mean unwanted tissue growth is still there. We keep checking until the hCG levels are back to normal. We ensure there's no return of this issue for a while after. Patients should steer clear of becoming pregnant during this time for at least six months. It helps to keep the hCG monitoring accurate.
2. Treatment for Malignant GTD or GTN
Malignant forms of GTD, such as invasive moles, choriocarcinoma, and placental-site trophoblastic tumors, require more advanced interventions.
Chemotherapy:
Chemotherapy is highly effective for treating malignant GTD, with cure rates exceeding 90% even in advanced cases.
Single-Agent Chemotherapy:
Simple cases with low risk get treated using one chemo drug, such as methotrexate or actinomycin-D. These drugs aim right at trophoblastic cells. This way, other tissues don't get as harmed.
Multi-Agent Chemotherapy:
For cases that carry high risks, it's often beneficial to use mixed treatment plans. One such plan is EMA-CO. It includes etoposide, methotrexate, actinomycin-D, cyclophosphamide, and vincristine
Book an Appointment
Surgical Interventions
Hysterectomy:
Patients who are done having kids or having uncontrolled bleeding/infection or those not responding to chemo might need their uterus taken out. This, a hysterectomy, wipes out the disease where it started and stops more problems.
Surgery for Metastases:
When dealing with spreading diseases, sometimes doctors remove growths from organs like the lungs or brain. They do this to make conditions better or handle problems like bleeding.
Radiation Therapy:
Often, radiation isn't the first choice, but it’s sometimes used. Even in tough spots like the brain or liver, where treatment can be tricky.
Prognosis of Gestational Trophoblastic Disease
Good news, though! If GTD is caught early and treated right, the outlook is usually great!
- Type of GTD: Benign forms, such as hydatidiform moles, have nearly a 100% cure rate. Malignant types like choriocarcinoma respond well to chemotherapy, often achieving complete remission.
- Extent of Disease: Localized GTD has an excellent prognosis, while metastatic cases require more aggressive therapies but still have high cure rates with modern treatments.
- Patient’s Health: Timely intervention, regular monitoring, and overall patient health significantly impact recovery outcomes. Most patients recover fully, and fertility is often preserved.
Preventive Measures and Risk Reduction
Gestational Trophoblastic Disease (GTD) isn't 100% preventable. However, some steps can lower its likelihood and catch it early.
- Regular Prenatal Care: It's key to have regular check-ups and ultrasounds when pregnant. This helps spot irregularities, like molar pregnancies, early enough for helpful intervention.
- Genetic Counseling: If a woman's had molar pregnancies or recurrent GTD, a chat with a genetics counselor can be helpful. It helps her understand her chances and gives advice for future pregnancies.
- Balanced Nutrition: Eating enough necessary nutrients, particularly vitamin A, is important. It boosts reproductive health and can help lower chances of abnormal placental growth.
- Awareness of Risk Factors: For women who are over 35 or under 20, or those who've had GTD before, staying alert is critical. Always share your medical background with your healthcare providers.
Book an Appointment

Why Choose Dr Sarita Kumari for the Gestational Trophoblastic Disease Treatment in India?
In the area of dealing with gestational trophoblastic disease (GTD) in India, Dr. Sarita Kumari clearly distinguishes herself as a prime authority. Here's the reason patients favor her:
1. Unparalleled Qualifications and Training
Dr. Sarita Kumari has impressive educational achievements. She received all her MBBS, MD, and MCh degrees in Gynecological Oncology from the respected AIIMS, New Delhi. This background proves her extensive understanding and skills in treating gynecological cancers, including GTD.
2. Global Expertise
She's so committed to being the best, she didn't just train in India. She also studied at international schools to learn about modern practices and improved treatments for tricky women's health issues like GTD.
3. Renowned Genetic Counselor
Dr. Sarita ranks amongst the top doctors for Gestational Trophoblastic Disease in India, her focus being on genetic guidance for women's cancers. Her skill gives a guarantee of precise danger evaluation and customized treatment design for patients.
4. Comprehensive Care
People appreciate Dr. Sarita. She's caring and focuses on her patients. She doesn't deal with only health issues. She also takes care of the feelings and worries of the patients and their loved ones.
5. Accessibility and Convenience
If you're looking for local genetic testing advice, Dr. Sarita is a good choice. Offering both worldwide knowledge and easy availability in India, she's a dependable source.
Though Gestational Trophoblastic Disease (GTD) isn't common. It needs quick spotting and taking care of it. Thanks to strides in medicine, most people with GTD now have a solid chance to recover. The keys? Knowing about it, finding it early, and getting overall treatment.
Suppose you or a person you're close with shows signs hinting at GTD. It's key to get medical help right away. Correct Gestational Trophoblastic Disease treatment in India and care can lead straight to a hopeful result


